by Mark Houston, MD and Sara Gottfried, MD
| The top five cardiovascular risk factors are hypertension, diabetes mellitus, dyslipidemia, obesity and smoking. Numerous clinical trials suggest that we have reached a limit in our ability to lower the incidence of coronary heart disease with conventional diagnostic evaluation, prevention and treatment strategies for these risk factors. About 80% of heart disease (heart attacks, angina, coronary heart disease and congestive heart failure) can be prevented by optimal nutrition, optimal exercise, optimal weight and body composition, mild alcohol intake and avoiding smoking. Statistics show that approximately 50% of patients continue to have coronary heart disease or myocardial infarction despite presently defined normal levels of the five risk factors listed above. This is often referred to as the ‘CHD gap’. Novel and more accurate evaluations of the top five risk factors are required, as well as translating the numerous traumatic insults from the environment that result in vascular endothelial responses (inflammation, oxidative stress and immune vascular dysfunction). The concept of translational cardiovascular medicine is critical and can be accomplished by utilizing advanced and updated cardiovascular risk scoring systems, new and redefined cardiovascular risk factors and biomarkers, micronutrient testing, cardiovascular genetics, nutrigenomics, metabolomics, genetic expression testing and noninvasive cardiovascular testing. |
Introduction
According to the World Health Organization, coronary heart disease is the number one cause of death in the United States and worldwide.1 Coronary heart disease is the most common form of cardiovascular disease, afflicting over 7 million people, and approximately 50% of the people who die from heart disease experience no previous symptoms.2,3 Unfortunately, we have not changed mortality from coronary heart disease in the last two decades.1 It seems we have reached a limit on our ability to reduce coronary heart disease and myocardial infarction.4 So the question we must ask the medical community is “Why? What are we doing wrong?” We have access to all the greatest technologies and drugs, we can measure anything and everything, and yet the change in rates of coronary heart disease is flat. Why are we not reducing the risk of coronary heart disease and myocardial infarction?
Definition of CHD risk factors
When we explore possible reasons why this is the case, we discover that there is a huge gap between what should be happening and what actually happens. If you go into a typical medical office, they will tell you the five major risk factors for coronary heart disease (CHD) are hypertension, dyslipidemia, diabetes, obesity, and smoking. Traditional medicine is focused on getting the LDL cholesterol down, getting the blood pressure down and controlling diabetes. However, the problem begins with not defining or measuring the top five risk factors correctly. Statistics show that approximately 50% of patients continue to have CHD or myocardial infarction (MI) despite presently defined ‘normal’ levels of the five risk factors listed above.5,6 This is often referred to as the ‘CHD gap’.7 Novel and more accurate definitions and evaluations of these top five risk factors are required, such as 24 h ambulatory blood pressure (ABM) results, advanced lipid profiles, redefined fasting and 2 hour dysglycemia parameters, a focus on visceral obesity and body composition and the effects of adipokines on cardiovascular risk.8
The second problem is, there are not only 5 risk factors for CHD. More than 400 CHD risk factors have been defined.6 That means there are 395 coronary heart disease risk factors that are not being measured, addressed, or treated. In practice, we can divide these into major categories and look at the top 25 modifiable risk factors. Even if you just addressed those top 25, you would have a huge impact on coronary heart disease risk.9 Examples of non-traditional modifiable risk factors that can be measured include fasting blood sugar with an insulin level, homocysteine levels, and inflammatory markers like C-reactive protein or interleukins. As previously discussed, measuring toxins and pesticides or measuring infections are also considered risk factors for a dyslipidemic response, and are related to CHD and MI.10,11
New CHD Model
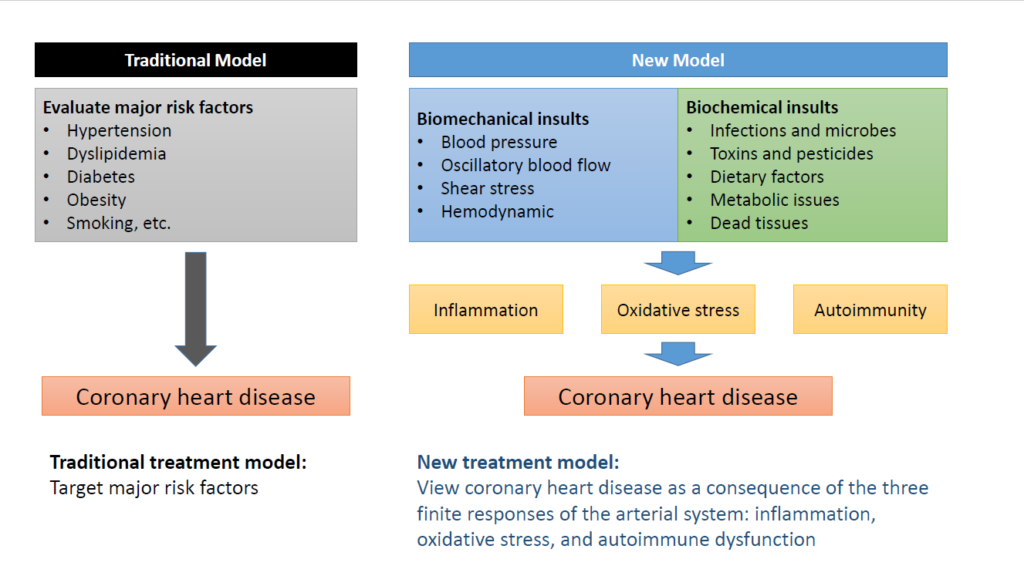
Once practitioners begin defining and measuring the risk factors correctly, the CHD model is totally revolutionized. The new model is similar to the model previously discussed with hypertension and lipids. There are two big groups of insults that damage the coronary arteries. Group one is biomechanical—like blood pressure, or oscillatory blood flow. The other group is biochemical. That’s everything else you can think of- infections, microbes, toxins, pesticides, lipids, homocysteine, metabolic issues, dead tissue, bacteria, you name it. These two pathways define the infinite insults. Biochemical insults come in and attach to receptors on the coronary artery. These receptors tell the artery that the substance is either foreign or friendly and mount a signal transduction response that is either favorable or unfavorable.
In the acute setting, whatever’s coming in is contained and dealt with–end of story. But if you keep damaging the artery over and over again with the same insult, the body recognizes that as a chronic dysregulation. The body is doing what it is supposed to do, but in the process of trying to defend the artery from damage, it becomes the wounded victim. And that’s where we have to change the way we approach CHD. So once the receptors are stimulated, they end up with the same three finite responses that we had with blood pressure and with dyslipidemia: inflammation, oxidative stress, and immune dysfunction. Therefore, we can think of CHD as an inflammatory disease of the arteries, an oxidative stress disease of the arteries and an autoimmune disease.6,7,12 If you think of CHD in this way, your entire approach will be different (Figure 1).
Vascular Biology Approach
With this new approach to CHD, practitioners will start with measuring the top 5 risk factors correctly using 24 ambulatory blood pressure monitoring (ABM), advanced lipid testing, body composition analysis, proper measurement of blood sugar with insulin, HbA1C and all the things that look at the dysglycemic response in a continuum, and obviously, get them to stop smoking. Then the other 25 modifiable risk factors can be analyzed including homocysteine, oxidized LDL, inflammatory markers, oxidative stress markers, immune markers just to name a few.13 These risk factors can be combined with nutrigenomics, genetics and epigenetics to get a picture of a patient’s true risk. Treatment can now go beyond treating the risk markers and translate into an actual change in vascular health in the coronary arteries. This is called “translational vascular medicine” and helps practitioners ensure that therapy translates into modifiable vascular responses that reduce future risk for CHD and myocardial infarction.8 Therefore, the primary goal is a vascular biology approach. If you make the artery healthy, you are going to reduce the finite responses that contribute to CHD.
Non-invasive testing
There are noninvasive tests of the coronary arteries that help determine whether or not a patient’s risk factors are already causing arterial damage. Table 1 shows various noninvasive functional, structural and other tests that are available beyond a coronary arteriogram to determine a patient’s risk for coronary heart disease.
Table 1
| Functional Tests | Structural Tests | Other Tests |
| EndoPAT (endothelial dysfunction, augmentation index and heart rate variablity | Carotid IMT/duplex (intimal medial thickness) and plaque | Cardiac PET, SPECT |
| CAPWA (computerized arterial pulse wave analysis) | CT angiogram | FDG-PET/CT: vascular inflammation/plaque/biologic activity |
| HRRT- heart rate recovery time | Coronary artery calcium score | PET/CT/F-NA-F for coronary plaque/inflammation/morphology |
| EKG and treadmill test | Cardiac MRI | PET/MRI for coronary plaque morphology and inflammation |
| Cardiopulmonary exercise test | ECHO: rest and exercise | Intravascular ultrasound |
| Magnetocardiography | Ankle brachial index: rest and exercise | Coronary angiogram |
CT- computed tomography; EKG- electrocardiogram; FDG-PET- fluorodeoxyglucose-positron emission tomography; IMT- intimal medial thickness; F-NA-F- sodium fluoride; MRI- magnetic resonance imaging; SPECT- single-photon emission computed tomography
First, it is important to know if the arteries are functionally abnormal. If the nitric oxide is low, and they’re constricted, it is non-obstructive coronary heart disease—also called Prinzmetal’s angina.14 The other form is obstructive coronary heart disease with a plaque. The process of learning to treat coronary heart disease is not only making the blood vessel healthy, but also recognizing whether one of three types of plaque are present and doing something to stabilize and possibly reverse it so it doesn’t rupture. There’s obstructive plaque that is “stable,” meaning it’s not likely to rupture. There’s obstructive plaque that is not stable which is called “vulnerable plaque,” where all the lipids, macrophages and inflammatory tissue are in a lipid core with a very thin fibrous cap. If all that gets into the lumen of the coronary artery, it causes a thrombus. That’s an acute myocardial infarction. The third, which has just been recently recognized, is called “erosive plaque.”15 It’s a different kind of non-obstructive plaque. The containment of the plaque is very different and slowly erodes through the fibrous layer. In approximately 30% of patients who die from heart attacks, more often women, there is just an erosion or ulceration of the plaque surface, rather than a full rupture that leads to clot formation in the coronary artery.16
Once the noninvasive testing is complete and you determine a patient is a candidate for medical therapy, it is time to start a treatment program. A medical therapy, whether it’s nutrition, nutraceutical, or drug, has to make a difference. But how do you know if your treatment program is actually changing the function of the coronary arteries or changing plaque growth and plaque stability in the coronary arteries? One novel approach is to utilize cardiovascular genetic expression testing. Cardiovascular genetic expression tests determine if cardiovascular genes have been turned on or off with a scoring system. Practitioners can use a combination of cardiovascular genomics, risk markers, genetic expression testing and noninvasive testing to evaluate therapy efficacy.
Let me give an example. A patient comes in with chest pain and completes all the testing and risk factor analysis. He only has 30% blockages in some of the larger arteries like the left anterior descending artery, right coronary artery or left circumflex artery. He is not a surgical candidate because the blockages are not severe enough. As a medical therapy candidate there are a lot of things that can be done to reduce the three finite responses, and that’s where you want to aim your therapy. At the same time you’re doing all that, you get a baseline gene expression test. The score ranges from 0-40 and your patient comes in with a score of 25, which is barely moderate risk.
You start your treatment program, wait six months, and repeat the gene expression test and some of the nonvascular testing like coronary calcium score, the EndoPAT, the computerized pulse wave analysis, all of which will tell you about endothelial dysfunction and structure of the coronary arteries. Let’s suppose the score drops from 25 to 20, which indicates the treatment has reduced the finite responses because that tests measure inflammation, oxidative stress, and vascular immune dysfunction. You’ve successfully reduced the patient’s outcome for CHD and MI. Showing the patient that his therapeutic program is working is very motivational because once the patient sees his progress, he’s likely going to continue your program. And in fact, he’ll probably want to keep going to get it down even more. He may be motivated to turn off every single insult so he doesn’t have to get an angioplasty or coronary bypass graft 15 or 20 years from now. Now practitioners can have a real impact on reducing risk of CHD.
Conclusions
In summary, we’ve reached the limit of reducing CHD and MI in this country. If we wish to revolutionize the prevention and treatment of CHD, a new approach should be implemented in the clinical setting. The top five CHD risk factors, as presently defined, are not an adequate explanation for the current limited reduction in CHD or the ‘CHD gap’. Proper definition and analysis of the top five risk factors, evaluating the other 395 risk factors and downstream mediators should be included with measurement of the three finite responses of inflammation, oxidative stress and vascular immune dysfunction, micronutrient testing, cardiovascular genetics, nutrigenomics, metabolomics, gene expression testing and noninvasive vascular testing. Early detection coupled with aggressive prevention and treatment of all cardiovascular risk factors will diminish the progression of functional abnormalities, structural problems and clinical CHD. This will be achievable by using a combination of targeted, personalized and precision treatments with optimal nutrition and nutraceutical supplements coupled with optimal exercise, weight and body composition management and a reduction in tobacco use. Approximately 80% of CHD can be prevented with this approach.8
Citations
- Global health estimates 2016: Disease burden by cause, age, sex, by country and by region, 2000-2016. Geneva 2018.
- Benjamin EJ et al. Heart disease and stroke statistics-2017 update: A report from the american heart association. Circulation. 2017;135:e146-e603.
- Mozaffarian D et al. Executive summary: Heart disease and stroke statistics–2016 update: A report from the american heart association. Circulation. 2016;133:447-454.
- Yusuf S et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the interheart study): Case-control study. Lancet. 2004;364:937-952.
- Gerstein HC et al. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 2011;364:818-828.
- Wolf-Maier K et al. Hypertension prevalence and blood pressure levels in 6 european countries, canada, and the united states. JAMA. 2003;289:2363-2369.
- Houston MC. Nutrition and nutraceutical supplements in the treatment of hypertension. Expert Rev Cardiovasc Ther. 2010;8:821-833.
- Houston M. The role of noninvasive cardiovascular testing, applied clinical nutrition and nutritional supplements in the prevention and treatment of coronary heart disease. Ther Adv Cardiovasc Dis. 2018;12:85-108.
- Helfand M et al. Emerging risk factors for coronary heart disease: A summary of systematic reviews conducted for the U.S. Preventive services task force. Ann Intern Med. 2009;151:496-507.
- Houston MC. Role of mercury toxicity in hypertension, cardiovascular disease, and stroke. J Clin Hypertens (Greenwich). 2011;13:621-627.
- Houston MC. The role of mercury and cadmium heavy metals in vascular disease, hypertension, coronary heart disease, and myocardial infarction. Altern Ther Health Med. 2007;13:S128-133.
- O’Donnell CJ et al. Genomics of cardiovascular disease. N Engl J Med. 2011;365:2098-2109.
- Houston MC et al. Addressing the global cardiovascular risk of hypertension, dyslipidemia, and insulin resistance in the southeastern united states. Am J Med Sci. 2005;329:276-291.
- Keller KB et al. Prinzmetal’s angina. Am J Crit Care. 2004;13:350-354.
- Virmani R et al. Plaque rupture and plaque erosion. Thromb Haemost. 1999;82 Suppl 1:1-3.
- Arbustini E et al. Plaque erosion is a major substrate for coronary thrombosis in acute myocardial infarction. Heart (British Cardiac Society). 1999;82:269-272.
Mark Houston, MD, MS, FAHA, FASH, DABC is a highly recognized cardiovascular and hypertension specialist, serving as a physician at St. Thomas West Hospital in Nashville, where he holds several leadership positions including Director of the Hypertension Institute and Vascular Biology, Medical Director of Clinical Research, and Section Chief for the Division of Nutrition. Dr. Houston cofounded the Hypertension Institute, which is one of the leading institutes in the US for hypertension treatment. An American Society of Hypertension (ASH) specialist and Diplomate of the American Board of Cardiology, Dr. Houston is also a Fellow of the American Society of Hypertension (FASH), the American Heart Association (FAHA), Internal Medicine (ABIM), American College of Nutrition (FACN) and Anti-Aging Medicine (ABAARM). Dr. Houston received his medical degree from Vanderbilt University. He also obtained two master’s degrees, in Human Nutrition and Metabolic Medicine and Human Nutrition, from the University of Bridgeport and University of South Florida, respectively.
Sara Gottfried, MD is a board-certified gynecologist and physician scientist. She graduated from Harvard Medical School and the Massachusetts Institute of Technology and completed residency at the University of California at San Francisco. Over the past two decades, Dr. Gottfried has seen more than 25,000 patients and specializes in identifying the underlying cause of her patients’ conditions to achieve true and lasting health transformations, not just symptom management.
Dr. Gottfried is a global keynote speaker who practices evidence-based integrative, precision, and Functional Medicine. She recently published a new book, Brain Body Diet and has also authored three New York Times bestselling books: The Hormone Cure, The Hormone Reset Diet, and Younger.