by Christopher Moulton, PhD
Introduction
At this point in the pandemic, clinicians are aware of the most typical symptoms related to COVID-19 infection: persistent fever, a dry cough, and shortness of breath. However, to a lesser extent a variety of other symptoms have been reported in coronavirus-afflicted patients, including fatigue, myalgia, rhinorrhea, and a sore throat.1 Notably, the first documented American patient with the novel coronavirus experienced nausea and diarrhea concurrent with cough, which occurred prior to any respiratory distress.2 Two recent publications have begun to characterize the prevalence of gastrointestinal symptoms in COVID-19 patients from Wuhan, China.
Research reports
In the first of these, Pan et al. conducted a cross-sectional evaluation of 204 patients (mean age 52.9 ± 16.0 years) from three hospitals in the Hubei province.3 All cases were confirmed positive for COVID-19 by reverse transcription-polymerase chain reaction (RT-PCR), and measures included chest CT imaging and routine labs including complete blood count, clinical chemistry, coagulation markers, and urinalysis. Slightly more than half of the patients admitted to the hospital (n = 103) presented with at least one gastrointestinal symptom, including anorexia (n = 81), diarrhea (n = 35), vomiting (n = 4), and abdominal pain (n = 2). Of these, 97 had developed respiratory symptoms concurrently with digestive symptoms, while 6 patients presented with only digestive symptoms but no respiratory symptoms.
Patients with gastrointestinal symptoms had a longer time from onset of first symptoms to hospital admission in comparison to those without gastrointestinal symptoms (9.0 days vs. 7.3 days). Although there are numerous plausible explanations for this difference, it is possible that patients experiencing gastrointestinal distress may not have suspected COVID-19 infection in the absence of any hallmark respiratory symptoms, and therefore delayed hospital entry for care. The authors noted qualitatively that as the severity of the disease advanced, the digestive symptoms became more pronounced. Patients with digestive symptoms had higher levels of liver enzymatic activity (ALT & AST) and lower monocyte counts than patients without digestive symptoms. There were no significant differences in mortality, days in the ICU, or time to discharge between the two groups.
Similarly, Han et al. conducted a retrospective analysis of 850 patients admitted to a single Wuhan hospital with COVID-19 infection confirmed by RT-PCR from nasal and pharyngeal samples.4 Patients with mild severity were selected (n = 206; mean age 62.5 years), as defined by lack of dyspnea, no other signs of respiratory distress, and SpO2 ≥ 93% at rest. All patients in this study were ultimately discharged from the hospital after viral clearance. Cases were identified presenting with one or more gastrointestinal symptoms (n = 117), which included nausea, diarrhea, and vomiting, and compared to controls with only respiratory symptoms but no gastrointestinal symptoms (n = 89). The case cohort was further subdivided into patients who had digestive symptoms only (n = 48) and patients with digestive AND respiratory symptoms (n = 69). Descriptive clinical features were similar among the three groups, although dyspnea, fatigue, and muscle soreness were more common in the digestive + respiratory group than in the respiratory-only group. Stool samples were collected in a subgroup of 22 patients from the overall cohort to assess for COVID-19 viral RNA via RT-PCR.
Sixty-seven patients presented with diarrhea, and 13 of these experienced diarrhea as the first symptom and prior to onset of any respiratory symptoms. The remaining 54 patients developed diarrhea within 10 days of the onset of respiratory symptoms. Diarrhea was more common in women than men (65.7% vs 51.1%), lasting from 1-14 days, with an average duration of 5.4 ± 3.1 days. Similar to Pan et al., patients with gastrointestinal symptoms had a longer gap between onset of symptoms and hospital entry than those with only respiratory symptoms (16.0 ± 7.7 days vs. 11.6 ± 5.1 days). The total time between symptom onset and viral clearance was longest in those with digestive plus respiratory symptoms (42.0 days), shortest in those with only respiratory symptoms (33.5 days), and intermediate with only digestive symptoms (40.9 days). Twelve of 22 patient’ stool samples tested positive for COVID-19 RNA (54.5%); patients with gastrointestinal symptoms were more likely to test positive for fecal virus (73.3%) than those without (14.3%).
Is the gut involved in COVID-19 infection and Transmission?
These two studies suggest that digestive symptoms are perhaps an underrecognized phenomena. This is particularly concerning as it relates to so-called “asymptomatic carriers”—does “asymptomatic” presume only respiratory factors? Should COVID-19 be automatically ruled out for a patient with four days of persistent diarrhea but no other complaints? Further, gastrointestinal symptoms may be indicators of advancing clinical severity; even in clinically resolved cases, digestive symptoms were associated with a longer hospital stay.4 That Han et al. identified viral RNA in stool at a rate approximately five times greater in patients with gastrointestinal involvement is consistent with reports that nearly a quarter of stool samples test positive for SARS-CoV-2 while concurrent nasopharyngeal samples test negative.5,6 As an illustrative case report from March 25th, a Chinese woman was admitted with respiratory symptoms and hallmark “ground glass” opacities upon chest CT scan, yet a pharyngeal sample tested negative for COVID-19 via RT-PCR. However, the same test administered on a fecal sample the following day tested positive.5
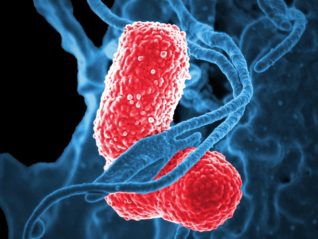
At the very least, these findings indicate that gastrointestinal tissues are markedly involved in the progression of a subset of clinical cases, and conceivably the gut could be actively involved in viral pathogenesis. At a molecular level, the SARS-CoV-2 virus is known to utilize binding to ACE-2 receptor for entry into target cells of the host,7 and although much attention has been paid to ACE-2 receptor density in the pulmonary epithelium,8 these receptors are relatively more abundant in intestinal epithelial cells, spanning from the duodenum, jejunum, and ileum to the cecum and colon.9
Live COVID-19 virus has recently been identified by electron microscopy in fecal samples that were RT-PCR positive,10 adding to concerns that COVID-19 may be transmissible via the fecal-oral route. However, this hypothesis has not yet been confirmed clinically, and ongoing research is under way to investigate this possibility further.11 Interestingly, several research groups are utilizing surveillance of sewage waste to monitor community infection rate in the absence of widespread testing;12 thus far COVID-19 has been identified in wastewater streams in the United States, Netherlands, and Sweden.13
Connecting gut and immune function
It’s been understood for over 20 years that at least two-thirds of all immune cells are resident in the intestine and surrounding splanchnic tissues,14 and more advances have revealed the complex influence of gut microbes on immunostasis.15 Dysbiosis or reduced microbial competition by commensal microbes can alter the network of signaling molecules within the intestinal mucosa, potentially hampering innate and adaptive immune responses to pathogens, thereby elevating susceptibility to infectious diseases.16 These effects may be, in part, mediated through microbial production of short-chain fatty acids (SCFAs), which have been show in vivo to favorably regulate CD8+ T cells17 and protect against viral infections by activating interferon-β signaling pathways.18
Adequate consumption of fiber-rich foods including fruits and vegetables may support host immune function by stimulating microbial production of SCFAs and facilitating maintenance of gut barrier function.19 A landmark study in 2016 utilized a germ-free mouse model to demonstrate that deprivation of dietary fiber resulted in a diminished mucus protective layer, as “hungry” microbial communities shifted to consume mucus glycoproteins as an energy substrate. As a result, these animals demonstrated increased intestinal permeability and became more susceptible to lethal colitis via Citrobacter rodentium.20 Research on the emergent phenomenon of the gut-lung axis, whereby gut microbiota crosstalk with the lung immune system and resident microbes, may reveal novel approaches to address respiratory infections through nutrition-based interventions.21
Key takeaways
- Keep an eye out for gastrointestinal symptoms, particularly sustained diarrhea, as a sign for possible COVID-19 infection
- Encourage good sanitation and hygiene practices, as fecal-oral transmission of the novel coronavirus has not been ruled out
- A fiber-rich diet containing a variety of plant-based foods may support immune homeostasis through eubiosis
Critical note: there are no studies directly investigating the effect of any foods or fiber on the immune response to the novel coronavirus. There is no clinical evidence demonstrating that any foods or fiber helps prevent, reduce, or treat COVID-19 infection.
Citations
- April 8, 2020 Q&A on coronaviruses (COVID-19). https://www.who.int/news-room/q-a-detail/q-a-coronaviruses. Accessed April 11, 2020.
- Holshue ML et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929-936.
- Pan L et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020. (Epub ahead of print).
- Han et al. Digestive symptoms in COVID-19 patients with mild disease severity: Clinical presentation, stool viral RNA testing, and outcomes. https://journals.lww.com/ajg/Documents/COVID19_Han_et_al_AJG_Preproof.pdf.
- Chen L et al. COVID-19 disease with positive fecal and negative pharyngeal and sputum viral tests. Am J Gastroenterol. 2020.(Epub ahead of print).
- Gu J et al. COVID-19: Gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology. 2020;S001650852030281X.
- Li W et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426(6965):450-454.
- Zhang H et al. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. March 2020:1-5.
- Harmer D et al. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532(1-2):107-110.
- Wang W et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020.
- Hindson J. COVID-19: faecal–oral transmission? Nature Reviews Gastroenterol Hepatol. 2020:1-1.
- Lodder W et al. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterol Hepatol. 2020;0(0).
- Mallapaty S. How sewage could reveal true scale of coronavirus outbreak. Nature. 2020;580(7802):176-177.
- Kagnoff MF. Immunology of the intestinal tract. Gastroenterology. 1993;105(5):1275-1280.
- Lazar V et al. Aspects of gut microbiota and immune system interactions in infectious diseases, immunopathology, and cancer. Front Immunol. 2018;9:1830.
- van den Elsen LW et al. Embracing the gut microbiota: the new frontier for inflammatory and infectious diseases. Clin Transl Immunology. 2017;6(1):e125.
- Luu M et al. Regulation of the effector function of CD8 + T cells by gut microbiota-derived metabolite butyrate. Scientific Reports. 2018;8(1):1-10.
- Antunes KH et al. Microbiota-derived acetate protects against respiratory syncytial virus infection through a GPR43-type 1 interferon response. Nature Communications. 2019;10(1):1-17.
- Simpson HL et al. Review article: dietary fibre-microbiota interactions. Aliment Pharmacol Ther. 2015;42(2):158-179.
- Desai MS et al. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. 2016;167(5):1339-1353.e21.
- Enaud R et al. The gut-lung axis in health and respiratory diseases: A place for inter-organ and inter-kingdom crosstalks. Front Cell Infect Microbiol. 2020;10:9.
Christopher Moulton, PhD is the Therapeutic Platform Lead for Cognition & Special Projects at Metagenics. Dr. Moulton endeavors to develop innovative, science-based solutions for practitioners to improve and enhance the well-being of their patients. Relatedly, he engages with the scientific & medical communities to better understand the potential of personalized nutrition to advance health care. Dr. Moulton completed a PhD in Nutritional Sciences at the University of Illinois in Urbana-Champaign. He also holds a Master’s degree in Exercise Physiology and a Bachelor’s degree in Biochemistry. Prior to joining Metagenics, Dr. Moulton managed the Center for Nutrition, Learning, & Memory, a public-private partnership focused at the intersection of nutrition & neuroscience.